Your assigned neurosurgeon and his nurse will meet with you by video to review your second opinion results. He will answer your questions. If surgery is needed, and you are considering surgery in the United States, be sure to let him know.
Read below to gain a detailed understanding of the surgery process.
Abstract
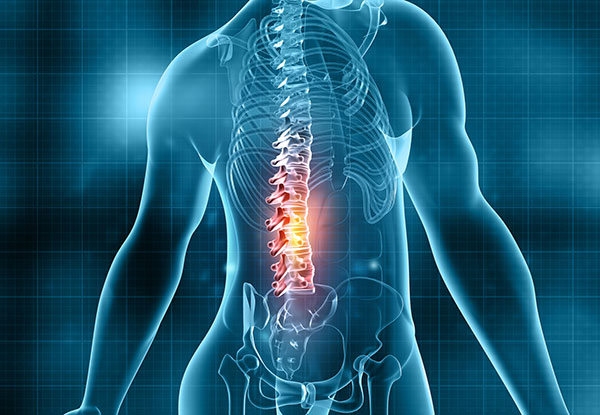
Back surgery, also known as spine surgery, aims to relieve pain, improve function, and address structural issues in the spine. Common reasons for back surgery include herniated discs, spinal stenosis, degenerative disc disease, scoliosis, and fractures.
Types of Back Surgery
Pre-surgery Activities
The Surgery
Post-surgery Activities
Potential Risks and Complications
Conclusion
Back surgery can significantly improve quality of life by alleviating pain and restoring function. Thorough preoperative evaluation, meticulous surgical technique, and comprehensive postoperative care are essential for successful outcomes. The multidisciplinary approach involving surgeons, anesthesiologists, physical therapists, and other specialists ensures the best possible results for the patient.
Please be aware that the services offered on this platform are with U.S. physicians via a virtual 2nd opinion service. Diagnosis may differ when the physician has had the opportunity to provide an in-person examination. The absence of the in-person examinations can affect the accuracy of the diagnosis and resulting opinion. Please also be aware that a virtual 2nd opinion will not establish a provider-patient relationship. The provide patient relationship can only be established when the patient signs a consent to treatment form in the physician’s physical clinic location in the United States.