If you are considering traveling to the United States for surgery and recovery, our medical concierge or your personal caregiver will be responsible for coordinating all activities.
Additionally, the surgeon and his nurse you meet in your second opinion telemedicine can answer any additional questions you have about pre-surgery and post-surgery activities.
Abstract
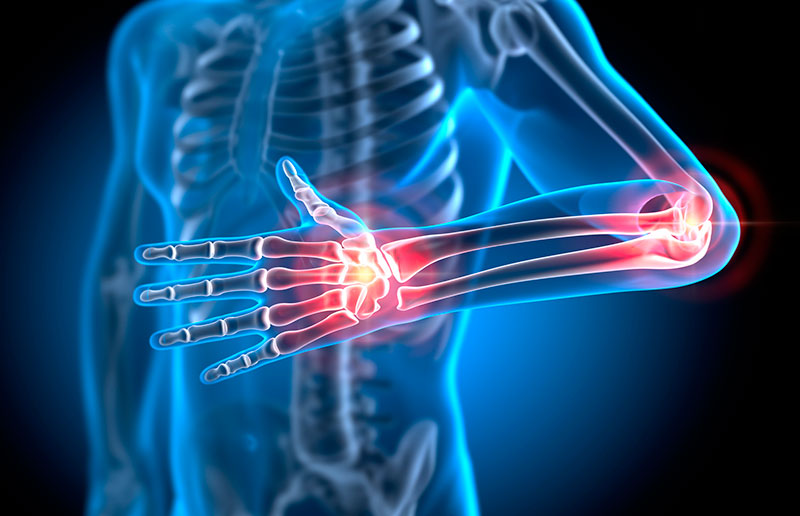
Arthritis surgery relieves pain, improves joint function, and enhances the quality of life for individuals with severe arthritis that doesn’t respond to conservative treatments. Arthritis can affect joints, including the knees, hips, shoulders, hands, and feet. The specific type of surgery depends on the affected joint and the extent of the arthritis.
Types of Arthritis Surgery
Pre-Surgery Preparation
The Surgery
Post-Surgery Recovery
Expected Outcomes
Conclusion
Arthritis surgery is a highly effective procedure for treating severe arthritis that doesn’t respond to conservative treatments. Proper pre-surgery preparation and diligent post-surgery care are crucial for optimal outcomes. Following your surgeon’s recommendations and engaging in regular physical therapy are key components of a successful recovery.
Please be aware that the services offered on this platform are with U.S. physicians via a virtual 2nd opinion service. Diagnosis may differ when the physician has had the opportunity to provide an in-person examination. The absence of the in-person examinations can affect the accuracy of the diagnosis and resulting opinion. Please also be aware that a virtual 2nd opinion will not establish a provider-patient relationship. The provide patient relationship can only be established when the patient signs a consent to treatment form in the physician’s physical clinic location in the United States.